This article introduces several sterilization methods for sterile medicines: moist heat sterilization, dry heat sterilization, radiation sterilization, ethylene oxide sterilization and sterilization filtration, and studies the sterilization principles and effects of various sterilization methods. Factors, advantages and disadvantages, and products suitable for sterilization, etc., and through the sterilization method of solution dosage form products and dry powder products or semi-solid and non-solution dosage forms, the decision tree is used to discuss the sterilization decision-making method of sterile drugs.
1 Overview Of Sterilization Of Sterile Drugs
Sterilization method refers to the method of killing or removing all surviving microbial propagules or spores by physical and chemical methods to make the sterilized items sterile. In the production of sterile drugs, the prevention of endotoxin contamination and microbial contamination has always been the focus of attention of regulatory agencies and manufacturers. Sterilization of sterile drugs is to remove or kill spores and microbial propagules in the drug, so as to ensure the safety of the drug preparation itself, and at the same time ensure the stability of the drug and its clinical therapeutic effect, so these sterile drugs It is of great significance to ensure the quality of medicines that the production enterprises adopt appropriate sterilization methods.
2 Introduction To Sterilization Methods Of Sterile Drugs
2.1 Moist Heat Sterilization
Moist heat sterilization refers to the use of high-pressure steam or other thermodynamic sterilization methods to kill microorganisms in articles in a sterilizer. Moist heat sterilization is one of the most widely used and most effective methods in thermodynamic sterilization, which has the characteristics of fast conduction, strong penetrating power, and stronger sterilization ability. At present, this method is included in “Chinese Pharmacopoeia”, “US Pharmacopoeia”, “European Pharmacopoeia”, and GMP regulations of various countries.
Principle: Moist heat sterilization is to denature the nucleic acid and protein of microorganisms by means of moist heat, thereby causing their death. This kind of denaturation is that the hydrogen bond in the molecule is first split, and then the internal structure of nucleic acid and protein is destroyed, so that its original function is lost, and the purpose of sterilization is achieved.
Factors affecting the effect of moist heat sterilization include:
① The length of time required for sterilization is related to the number of microorganisms in the initial sterilized object, so according to the first-order kinetic equation, the number and type of microorganisms in the sterilized object directly affect the sterilization effect. bacteria effect.
②In general, the heat resistance of microorganisms is the best in neutral solutions, poor in alkaline solutions, and worst in acidic solutions, so the pH of the sterilization solution is also an influencing factor for the sterilization effect.
③ The nature of the sterilized substance. If the solution contains nutrients such as amino acids and sugars, the microorganisms will be protected by these nutrients, thereby enhancing their heat resistance.

④ The penetration of dry hot air and superheated steam is much worse than that of saturated steam, so the saturation of steam is another factor affecting the sterilization effect, and saturated steam should be used for sterilization as much as possible.
2.2 Dry Heat Sterilization
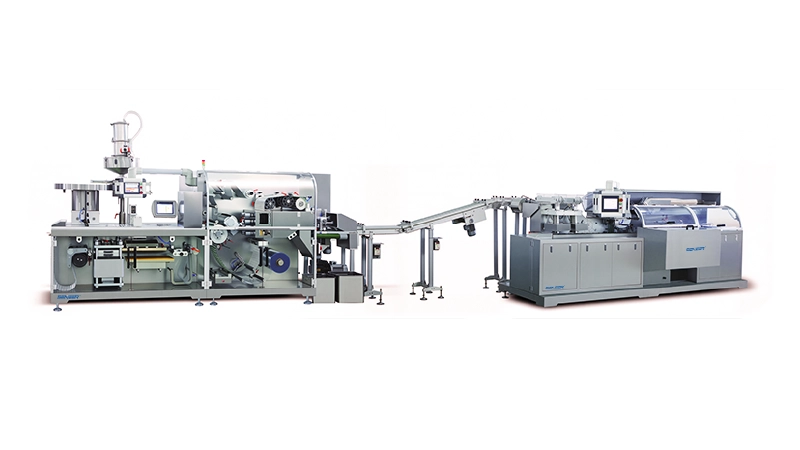
Dry heat sterilization is a method of killing microorganisms by non-specifically oxidizing biopolymers such as deoxyribonucleases and microorganisms at high temperatures. According to the different ways of use, dry heat sterilization equipment can be divided into continuous type and intermittent type. For example, tunnel type sterilization oven is continuous type, which is used for the sterilization of vials or ampoules; while dry heat sterilization cabinet is Intermittent type, can be used for sterilization of equipment parts and metal utensils to remove heat source.
The thermodynamic principle of dry heat sterilization is similar to that of moist heat sterilization, and the killing of microorganisms also conforms to the logarithmic principle under certain sterilization conditions.
Dry heat sterilization can be considered for high temperature-resistant powder chemicals, some metal equipment, oils and utensils that do not need moisture penetration, and glass and other high-temperature resistant items, but it is not suitable for most pharmaceuticals, plastics and For rubber sterilization, dry heat sterilization can also remove heat source. For example, in the production workshop of sterile pharmaceutical injections, some appliances in the B-level and C-level clean areas can be sterilized by electric heating through a double-door dry heat sterilizer.
2.3 Radiation Sterilization
Radiation sterilization is a sterilization method that uses ionizing radiation to kill microorganisms. The electromagnetic waves used for sterilization include microwaves, ultraviolet rays, γ-rays, and X-rays. At present, radiation sterilization mostly uses gamma rays emitted by 60Co sources.
The principle of the radiation sterilization process: In a specially designed device, the product is exposed to gamma rays produced by cobalt 60 (60Co) radionuclide, cesium 137 (137Cs) radionuclide, or electrons or X-ray beams, thereby achieving the method of killing microorganisms.
Radiation sterilization has the following advantages: ① Sterilization at room temperature, the temperature rise in the product sterilization process is small, and it is suitable for the sterilization of heat-sensitive biological products and drugs. ②The process is simple. Once the sterilization parameters are determined, time is the only adjustable factor, which is suitable for large-scale industrial production, saves energy, and does not pollute the environment. ③ Sterilize after packaging. Under the condition of airtight packaging, the product can maintain a sterile state for a long time. ④ The penetrating power of radiation is very strong, and its sterilization is also thorough, and it is not limited by the packaging and shape of the article. ⑤After irradiation, there is no radioactive residue and no side effects such as chemical toxicity in the product.
2.4 Ethylene Oxide Sterilization
Ethylene oxide sterilization is a relatively reliable low-temperature sterilization method. Ethylene oxide has an unstable three-membered ring structure and its small molecule characteristics, making it highly penetrating and chemically active. The common ethylene oxide sterilization process adopts a vacuum process, and generally 100% pure ethylene oxide or a mixed gas containing 40%~90% ethylene oxide (for example: mixed with carbon dioxide or nitrogen) can be used. When the positive pressure process is adopted, 8%~20% ethylene oxide is mixed with carbon dioxide gas. The product is sterilized in a pressurized chamber filled with sterilizing gas. The standard ethylene oxide sterilization process consists of 3 distinct stages: pretreatment, sterilization and desorption.
The principle of ethylene oxide sterilization: ethylene oxide is a broad-spectrum sterilant that can kill fungi, spores, viruses, bacteria and other microorganisms at room temperature; Alkylation of groups, carboxyl groups, etc., resulting in the death of microorganisms; it can also inhibit the biological enzyme activity of cholinesterase, cholinesterase, peptidase, phosphoactivase, etc.; ethylene oxide can also interact with RNA And DNA alkylation reaction leads to the inactivation of microorganisms.
2.5 Sterilization By Filtration
Sterile filtration refers to the process of removing microorganisms in a fluid through a filter, which should not adversely affect the quality of the product. Includes liquid and gas sterilizing filtration. The sterilizing filtration of liquids in the production of sterile pharmaceuticals generally adopts the pore size of the sterilizing filtration membrane not exceeding 0.22 μm, which can reach 107 CFU of Pseudomonas diminuta per square centimeter of effective filtration area under process conditions. General requirements.
For many terminally sterilized sterile products, filters are used to filter the products before filling before terminal sterilization to control the level of microbial contamination; for sterile products that cannot be terminally sterilized, such as some sterile water needles, Freeze-dried powder, etc. are filtered through sterile filtration before filling to achieve a sterile level. Consider reducing the risk of sterilizing and filtering. When one sterilizing filter can achieve the effect of sterilizing and filtering, add a second (or use multiple) sterilizing grade filters to ensure the effect of sterilizing and filtering. Such a setting, Often referred to as a “dual” or “redundant” setup.
3 Sterilization Decisions For Sterile Drugs
Sterilization of sterile drugs requires different methods to be selected according to the situation, generally considering the limitations of the purpose of use, the stability of the sterilized object, and the specific conditions in production. For example, glass containers are generally sterilized by dry heat, environmental facilities should be sterilized by chemical methods, rubber products and clothing are generally sterilized by moist heat, powders such as lactose and traditional Chinese medicine powder for subpackaging can be sterilized by radiation . Prepared products usually need to choose the appropriate sterilization method according to the characteristics of the product.