Contamination control is one of the core contents of drug production quality management. Based on the basic requirements of drug production quality management, this paper summarizes the key points of sterile drug contamination control strategies; , equipment and components, facility environment, materials, process, detection and prevention, etc. to refine and explain the typical and easily overlooked problems of pollution control, in order to provide guidance for the design and implementation of pollution control strategies for sterile drug manufacturers. The evaluation provides a reference for the production inspection of various sterile drugs.
Good manufacturing practice (GMP) aims to minimize the risks of contamination, cross-contamination, confusion, and errors during drug production. Pollution is the biggest threat to the quality of pharmaceuticals. Pollution control is an important part of the quality management of pharmaceutical production. The control of contamination such as microorganisms, pyrogens, and particles is the core point of the quality management of sterile pharmaceutical production. Both involve the contamination of sterile drugs. In view of the importance and particularity of contamination control of sterile drugs, some international drug inspection agencies divide drug inspectors into sterile drug inspectors and non-sterile drug inspectors. In recent years, in domestic and foreign drug inspections, relatively many problems have been found in the aspect of contamination control of sterile drugs, and some problems have caused great potential risks to the quality of drugs. Considering the above reasons, the European Medicines Agency (EMA) newly revised GMP Appendix for Sterile Drugs clearly puts forward the concept and requirements of pollution control strategies, and the International Pharmaceutical Inspection Cooperation (Pharmaceutical Inspection Cooperation) Scheme, PIC/S) GMP Appendix 2 Manufacture of Advanced Therapy Medicinal Products for Human Use (manufacture of advanced therapy medicinal products for human use) also clearly requires that production activities involving infectious virus vectors need to be based on written pollution control strategies and quality Risk management principles take isolation measures. Research on contamination control strategies of sterile drugs plays an important role in identifying and controlling contamination in advance for sterile drug manufacturers and ensuring product quality. Significance.

Part 1 Overview Of Sterile Drug Contamination And Contamination Control Strategies
Common sources of contamination for sterile pharmaceuticals mainly include microorganisms, cell debris (such as pyrogens, bacterial endotoxins), particles (such as glass, hair) and viruses, and their transmission media generally include gas, water, surfaces, materials, personnel, etc. Among them, personnel accounted for the highest proportion (about 35%). Contamination control strategy (CCS) is a series of planned control measures aimed at pollution sources such as microorganisms, pyrogens and particles based on the understanding of current products and processes to ensure product quality and process performance. Contamination control strategies are not a new requirement for sterile drugs, and the current drug GMP has clear regulations on pollution control requirements in all aspects of drug production.
At present, the new requirements for contamination control strategies in the EMA’s newly revised GMP appendix for sterile drugs only require companies to form a pollution control strategy document, linking all key control points and the effectiveness of control measures for contamination control of sterile drugs Detailed evaluation and elaboration. This pollution control strategy document should be included in the quality management system of the enterprise. Firstly, based on the principle of quality risk management (QRM), conduct a systematic and comprehensive design or evaluation of all pollution control elements, and establish or further improve control measures to eliminate risks. or reduce it to an acceptable level (CCS development, review and improvement, improvement); secondly, on this basis, compile pollution control strategy documents (CCS document compilation, which can be Refer to the attached template in ECA “How to develop and prepare pollution control strategy”); Finally, monitor and evaluate the established pollution control strategy (including the evaluation in the management review), take timely improvement measures and revise the corresponding pollution control strategy Documentation (CCS assessment). The pollution control strategy document is a quality system document similar to the verification master plan and the site master document. It involves the index of a large number of relevant quality management system documents on the basis of the overall analysis and introduction of the pollution control measures of various elements of sterile products. , to verify that all pollution control strategies and their elements have been effectively implemented.
Part 2 Analysis Of Key Points Of Contamination Control Strategies For Sterile Drugs
Drug pollution control is a systematic project, and the elements of pollution control in the sterile drug pollution control strategy can be classified and explained from different angles according to the actual situation. This study is mainly based on the quality management theory, classified from the six elements that affect drug quality, and combined with other drug regulatory inspection departments in my country and the world in recent years (mainly including the World Health Organization, the US Food and Drug Administration and the European Medicines Agency) The typical problems and new situations found in the inspection of sterile chemical drugs and biological products are analyzed around the key points of sterile drug contamination control strategies and problem examples.
2.1 Personnel Contamination Control
Personnel are the biggest source of pollution in pharmaceutical production. All personnel entering the clean production area and production-related personnel must undergo appropriate training and pass corresponding assessments (including training on microbiological knowledge and aseptic behavior norms) to ensure the standardized operation of personnel in the clean area, and establish hygienic standards and regulations for personnel entering the production area. Physical discomfort reporting system and appropriate health monitoring requirements, and monitor the standardization of behavior, specify the maximum number of people allowed to enter each clean room, equip clean work clothes that match the corresponding clean environment level and production operations, and formulate clean work clothes. , Sterilization, use times and deadlines and complete the corresponding verification. For those who enter the B-level clean area, they need to undergo clean dressing training and confirmation. Only after passing the assessment and confirmation can they enter the B-level clean area. Establish a list of personnel entering the B-level clean area, and conduct personnel qualification monitoring and regular reconfirmation. Personnel participate in the necessary aseptic process simulation tests as required to control the contamination caused by personnel to the greatest extent.
Some typical problems in personnel pollution control include:
①Irregular operations of personnel in the clean area, such as during the inspection, it is found that the operators gather and chat in the B-level clean area, fold their hands on their chests, walk quickly, make large movements, pick up from the floor, etc. Lifting objects, intruding the upper body or the whole arm into the Class A area, leaning against the production equipment or the wall, directly touching the control panel with fingers, directly turning the door handle to open and close the door, failing to sanitize hands after operation and before key operations , Kneeling and crawling into the transfer box to pass items, clean clothes touching the inner surface of the isolation door of the A-level area during the door opening and closing operation, and operators in the quality control clean area squatting and lying on the ground and other irregular behaviors.
② Irregular clean clothes, part of the body and skin of the operators in the B-level area is exposed, the repacking operators only wear one layer of gloves with short arms, and part of the clean clothes touch the ground, etc.
③ Some management regulations lack the support of verification data, and the implementation of the system is insufficient. For example, the maximum number of people entering the room, the maximum number of cleaning and sterilization times of clean clothes and the validity period, and the cleaning method of clean clothes have not been verified or confirmed correspondingly; during the execution of the program, the maximum number of people entering the room is not marked on site, and the number of people entering exceeds the specified maximum number. The cleaning and sterilization records of clean clothes are inconsistent with the number of sterilization sets in the same time period in the use records of sterilizers, and there are no problems such as clean clothes sterilization records.
④Relevant records are missing or the record information is incomplete, such as the list of personnel entering the B-level area has not been established, and the list of personnel entering the B-level area does not show the qualified time and validity period of personnel confirmation.
⑤ In other aspects, there is no effective system for reporting physical discomfort (for example, lack of reporting records, etc.), and the relevant regulations on hygiene for personnel entering the clean area are insufficient (for example, no consideration is given to limiting the number of people with skin diseases such as tinea pedis and severe dandruff) access) problem.
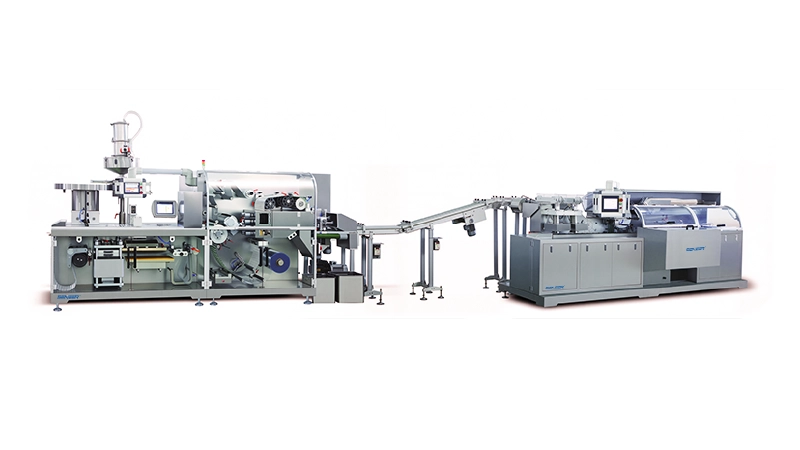
2.2 Equipment And Component Pollution Control
Equipment and components mainly include pharmaceutical production equipment (including pharmaceutical equipment, pharmaceutical water system, pure steam system, compressed air system, nitrogen system, etc.) and key components and seals in direct contact with pharmaceuticals (such as rubber stopper hoppers, silicone tubes, material And intermediate product containers, sealing rubber rings, etc.). Pharmaceutical production equipment needs to be reasonably designed and confirmed to ensure that it continues to meet the intended purpose. During the use of equipment, monitoring, cleaning, disinfection, sterilization, maintenance and repair should be done, and cleaning, disinfection and sterilization verification should be completed as required. The cleaning and sterilization methods, storage methods, maximum storage period, and allowable use times (if necessary) of key components and seals should be verified. Production equipment components that have a direct impact on contamination need to be monitored more frequently based on risk, such as high-efficiency filters in tunnel ovens, air filters in humid heat sterilizers, breathing valves on reaction tanks, and restricted access barriers. systems, RABS) operating gloves, etc. Select appropriate cleaners and disinfectants according to the conditions of the production equipment, carry out the effectiveness verification of disinfectants, and formulate scientific disinfection methods based on the verification results. For gases and liquids that require sterilization and filtration, corresponding sterilization and filtration verification should be carried out, and filter integrity testing, sterilization and use requirements should be implemented in daily production work. For key components (such as single-use systems, filter elements, etc.), it is necessary to strengthen the management of suppliers, and establish appropriate quality assurance requirements (involving safety, product compatibility, etc.), and evaluate the pollution of the single-use system based on the particularity of the system. risk.
Some typical issues in equipment and component contamination control include:
①Equipment design has potential pollution risks, such as the layout of one side of the filling line against the wall (<30cm) is difficult to effectively clean, the RABS of the filling line needs to open the door to replace the environmental monitoring plate, and the equipment assembly before filling takes too long Time, there are a large number of difficult-to-clean mesh holes on the surface of the equipment in the A-level area (and the company cannot prove that similar holes are conducive to the improvement of the air flow pattern), the rubber stopper hopper on the filling line cannot be removed for wet heat sterilization, etc.
② The monitoring frequency of the pharmaceutical water system is unreasonable, for example, the point of use of water for injection is only monitored once a month, and some point-of-use monitoring items lack bacterial endotoxin and microbial limits.
③The compressed gas in direct contact with materials/products is monitored only once every six months, and the monitoring frequency lacks effective risk assessment.
④ In the microbial monitoring of the equipment surface, there is a lack of microbial sampling methods for irregular equipment surfaces, the selection of sampling points lacks an effective risk assessment, the regulations for rotating/random surface microbial sampling positions are not established, and the operating gloves in the RABS are not checked every shift. Surface microbial sampling and testing.

⑤ Insufficient confirmation of key production equipment and insufficient daily monitoring, such as: the confirmation of autoclave equipment does not consider the worst condition, the life verification of chromatography medium is not carried out, and the confirmation of bottle washing machine does not include the position of the cleaning needle in the bottle It is stipulated that the integrity test of the breathing valve of the sterilizer is carried out once a month, but there is no regulation on the respirator assembly procedure before re-use. The bacterial endotoxin challenge test point is not placed inside the ampoule when the tunnel oven is confirmed, and the tunnel oven is only required to be carried out once a year. Integrity testing of high-efficiency filters and lack of reasonable explanations. The tunnel oven is required to conduct intervention monitoring every six months but the cooling section is not disinfected/fumigated before re-production. There is a lack of pressure difference monitoring and records between the tunnel oven cooling section and the filling line. , The design and monitoring of the reasonable pressure difference between the three different functional sections in the interior, etc.
⑥In terms of disinfectant selection and verification, there are unreasonable choices of disinfectants, no or insufficient verification of disinfectant efficacy (such as insufficient selection of surface materials, isolation of bacterial strains in unused environments, and only laboratory research, etc.). Disinfection operation regulations were formulated based on the effectiveness verification of disinfectants, and issues such as chromatography column disinfection and storage verification were not carried out.
⑦ Insufficient cleaning validation. There are deficiencies in limit standards, cleaning methods, worst-case conditions challenging tests, and cleaning validation sampling. The lack of analysis of the corresponding relationship between carbon standards and protein residues, and the lack of cleaning verification of non-special filter elements and silicone hoses, etc.
⑧ In terms of the sterilization and filtration system, there is no sterilization and filtration verification, the commissioned filter supplier to carry out the sterilization and filtration verification does not represent the actual filtration process, the integrity of the key filtration operation is not tested before use after sterilization, and the filter is complete. Insufficient investigation and handling of unqualified performance testing and lack of procedural regulations, long intervals between gas filter integrity testing and lack of effective evaluation, etc.
⑨Insufficient disinfection and sterilization of tools and appliances that directly contact materials and intermediate products, such as measuring cylinders, stainless steel barrels, stainless steel stirring rods and other tools that directly contact materials and intermediate products used in the preparation process, are cleaned, dried and stored in D-level clean areas , The influence of pyrogens and microorganisms has not been evaluated.
⑩The single-use plastic storage bags used to store intermediate products have not been inspected for integrity after use.
⑪The production equipment failed to carry out effective maintenance and repair, such as the deformation of the isolation door of the filling and stoppering machine, which caused it to not be completely closed.
2.3 Facility Environmental Pollution Control
The facility environment should be reasonably designed, laid out, verified, used and maintained based on the characteristics and cleanliness level requirements of the pharmaceuticals produced, and appropriate heating, ventilation and air-conditioning systems (HVAC) should be configured to ensure the pharmaceutical production environment Continue to comply with the corresponding cleanliness level requirements (including shielding systems, isolators, etc.), minimize potential contamination risks in the clean area (such as facility surfaces, interlayer probes, door opening and closing methods, pipeline layout, etc.), and establish a reasonable flow of people in the clean area Roads and logistics channels (including air locks, interlocking requirements, etc.), to ensure the range of pressure differences in areas with different cleanliness and areas with special control requirements, and to establish effective cleaning, disinfection, sterilization and monitoring methods for the facility environment in the clean area and frequency. Combined with the analysis of problems found in inspections in recent years, we need to pay special attention to two aspects in pollution control: one is the scientific and reasonable layout and design of the facility environment, such as the cleanliness level requirements for rooms directly connected to Class B clean areas, and the external environment. The requirements for internal observation in Class B areas, the design of clean area doors and opening and closing doors, the requirements for sterilization and filtration as close as possible to the filling line, and the design of airflow in the clean area; the second is the risk-based clean area environment Monitoring, environmental monitoring itself is also a kind of intervention behavior, so the more environmental monitoring is not the better, just like the research on verification, quality cost, etc., the key point is to find a scientific balance interval, and the number of monitoring points needs to be determined based on the risk principle (considering the area , people flow and logistics, production activity risk, layout, regulatory requirements, etc.), monitoring items (such as dust particles, planktonic bacteria, sedimentation bacteria and surface microorganisms, etc.), monitoring location (considering room layout, production process, early grid design, etc. , common locations such as the open area of the bottle in the filling line, the surface of the door handle, wall and curtain facility, the surface of the filling line, control panel, rubber stopper hopper, filling needle, filling line operating gloves, etc.), monitoring Frequency (should be able to detect potential system problems and potential contamination risks to products), and form a formal risk assessment document. During the formulation process, it is necessary to fully evaluate the possibility of adverse effects of the facility environment on product quality, and the worst case in actual production. Conditions, the rotation of daily monitoring points and the consideration of random monitoring points, the most difficult location to clean and disinfect, the impact of environmental sampling on the environment and products, and other factors, determine reasonable alert limits and action limits based on historical monitoring conditions, conduct regular review and Evaluation ensures the effectiveness of current environmental monitoring measures.
Some typical issues in facility environmental pollution control include:
①In terms of facility environment design, there are key production equipment (such as potting lines) that collect air from Class B indoors but do not evaluate the impact on air flow patterns, and do not evaluate the extended laminar flow in some Class B key operating areas in combination with actual production conditions. Necessity, the position design of the air supply and return air outlets in the clean room is difficult to ensure the air exchange in all areas of the room, the door of the B-level clean area has a position that is difficult to clean, and the door handle design requires the operator to directly switch and close the door with his hands There is a risk of lubricant falling off and polluting the environment, the level B operation area lacks external monitoring windows or effective surveillance cameras, the material channel in the B level key operation area is directly connected to the CNC area, and the product is not sterilized as close as possible to the distribution point Issues such as filtering and lack of reasonable assessment and formal assessment report.
② In terms of the use and maintenance of the facility environment, there are mainly problems of insufficient maintenance and monitoring of the use process. For example, it is found that the surface of the facility in the clean area is not smooth (damaged, glued, aged, sunken, raised, residual adhesive, etc.) Without considering the criticality of the production area and not based on the principle of quality risk management, the integrity test of the high-efficiency filter is only carried out once a year, and the interlock time setting of the logistics buffer room is not combined with the verification of the air-conditioning system. The room self-cleaning time and disinfectant are the smallest Action time etc.
③ In terms of clean environment verification, the air flow pattern test is only carried out under static conditions, the air flow pattern video cannot be provided, the content of the air flow pattern video display cannot prove the one-way flow, and the verification items are missing (such as not including surface microorganisms, Self-purification time, etc.), verifying the improper setting of environmental monitoring points and other issues.
④In terms of clean environment monitoring, it is mainly based on risk-based adequate assessment and design of monitoring locations, monitoring items, monitoring time, and monitoring frequency that are not combined with actual production and facility conditions. There is a risk of not being able to detect pollution in a timely manner. Some examples include: The surface microbiological monitoring project does not include the B-level area, and does not include all key locations for the A-level area (such as filling machine operating gloves, filling area and stoppering area), etc. The entire B-level area during production is only for one point in the filling room Carry out monitoring of planktonic and sedimentary bacteria, planktonic bacteria in A-level and B-level areas are only monitored before and after production starts, C-level areas are only monitored once a month, D-level areas are only monitored once a year, and clean environment is not monitored. Identify the microorganisms detected in the environment and take necessary environmental disinfection measures.
⑤Irregular operations of environmental monitoring, such as spraying disinfectant on the surrounding area of the plate near the sedimentation bacteria, the cover of the culture medium plate is not opened during the detection of planktonic bacteria, and the cover of the plate is placed obliquely on the plate to cover part of the sampling area of the plate during the detection of sedimentation bacteria wait.
⑥ Pollution risks related to other factory facilities, including smoke detectors, emergency escape doors, insect and rodent prevention measures, and paper records that produce fibers due to extensive use in Class B areas.
⑦The problems related to the disinfection of plant facilities are basically similar to those of equipment, and will not be described again.
2.4 Material Pollution Control
Materials mainly refer to the raw materials, auxiliary materials and internal packaging materials used in the production of pharmaceuticals. Suppliers of all materials (including manufacturers and distributors) should be confirmed and ensured to be in a continuous effective state (involving supplier assessment, supplier audit, qualified supplier management, etc.), and quality risk management should be based on the entire material supply chain According to the principle of identifying and controlling key links, strictly control all links of material acceptance, sampling, inspection, release, transfer and disinfection (including necessary verification), especially the microbial load, bacterial endotoxin and sterility requirements of materials, and at the same time, try our best Reduce the risk of material variation or damage, such as the transportation, transfer, cleaning, dry heat depyrogenation, filling, loading, unloading, and capping of fragile inner packaging materials such as vials and ampoules.
Some typical issues in material contamination control include:
① The risk control measures for the transportation and transfer of key materials are insufficient. For example, a sterile material for preparation is packaged in a single-layer plastic barrel and needs to be transported overseas for long distances. The risk of packaging damage during transportation is not identified and effectively controlled. Risk of adequate disinfection; lack of verification of disinfection procedures for materials entering the clean area, etc.
② There is a lack of effective facilities (such as a canopy with sufficient area) in the material receiving and receiving area of the warehouse to avoid the impact of bad weather on materials.
③ Pollution in the sampling process, there are sampling tools that have not been sterilized or lack of expiration date marks after sterilization, clean clothes for sampling are cleaned, sterilized and dried in the general experimental area of the QC laboratory, and effective measures are lacking to prevent pollution when sampling powder materials (especially activated carbon), etc.
④ No microbial or bacterial endotoxin testing items have been established in material standards, or the testing frequency of corresponding items has been reduced on the basis of lack of sufficient data and reasonable assessment.
⑤ For barreled materials that need to be tested for sterility, sampling and release are not carried out according to the established procedures, and they are not released for use in advance after the results of the sterility test.
2.5 Production Process Pollution Control

Manufacturers should conduct quality risk assessments for each sterile product production process based on the differences in the production processes of different types of products (such as non-terminal sterilization and terminal sterilization), carry out process verification (including continuous process validation), and at the same time evaluate the The method of sterilization, disinfection, virus removal or inactivation shall be verified, and effective measures shall be taken to avoid the risk of recontamination. In the whole production process, the possible pollution and pollution of starting materials, intermediate products, process transfer and storage, process control, aseptic operation and intervention of each process (including packaging links), sealing verification and testing, visual inspection, etc. The control measures are controlled, and the aseptic process simulation is carried out for the whole process of the aseptic production process of non-terminal sterilized products to ensure that the pollution in the production process is effectively controlled. In the production process, in addition to the pollution of microorganisms, cell debris and viruses, special attention should be paid to the pollution control of particulate matter (including glass, rubber, metal, ordinary fibers, plastic fibers and hair, etc.), especially the application and verification of fully automatic equipment and daily monitoring. Taking the pollution control in the production process of freeze-dried powder injection as an example, it can be cleaned and prepared before production, liquid medicine preparation, sterilization and filtration, filling, half-tamping and automatic box entry, freeze-drying, box capping, The pollution control measures in each process such as visual inspection, labeling and packaging are analyzed and controlled.
Some typical issues in manufacturing process contamination control include:
①In the control of intermediate products, there are situations where the microbial load test of the prepared intermediate products is not carried out before sterilization and filtration, and the testing standards are unreasonable.
② During process transfer and storage, the storage time of intermediate products has not been verified or the verification time is insufficient, the surface cleaning and disinfection procedures of intermediate products entering the B-level area through the CNC area have not been verified, and the glass bottles containing intermediate products in the aseptic production site are missing Status identification and other issues.
③In the aseptic process simulation, the main problem is that the actual production process and the whole process of aseptic operation cannot be effectively simulated. At the same time, there are also incomplete simulation test records, unreasonable design of intervention operations, and failure to conduct at least once every shift every six months as required. Aseptic process simulation, unconventional production that has not been produced for a year did not perform 3 consecutive successful aseptic process simulations when it was first started.
④ In the sealing verification and testing, the sealing of the screw-cap cryotubes used for cryopreservation of working cells has not been verified or tested; Carry out sealing verification or insufficient verification, etc.
⑤ During the light inspection process, the illuminance of the light inspection machine does not meet the standard requirements, the monitoring position of the illuminance of the light inspection machine does not include the actual light inspection area, and the rest time regulations of the light inspection personnel during the light inspection cannot guarantee the recovery of eye fatigue.
⑥ In the verification of virus removal/inactivation capabilities, if the verification plan for 37% formaldehyde inactivation disease lacks stirring speed and temperature information, and the virus aggregation test is not carried out before inactivation, the loading mode of inactivation virus verification is consistent with the inactivation virus in daily production. Inconsistent loading patterns, etc.
2.6 Requirements For detection in pollution control
Although the detection ability of sterility testing is low due to the statistical factors of the number of tests, take an intuitive calculation as an example: 100,000 injections were produced, of which 1,000 were contaminated (1% failure rate), 40 tubes were randomly selected for standardized sterility testing, and the probability of passing the sterility test was about 66.9%. The limitations of sampling testing are more obvious in sterility testing. Nevertheless, sterility testing still plays an important role in checking, especially when the batch contamination rate is greater than 15%, the probability of failure of sterility testing is greater than 99.8%. Further combining scientific sampling strategies can more effectively improve the effectiveness of sterility testing in contamination identification. Overall, testing plays an important role in pollution control, mainly including intermediate product testing, finished product testing, and trend analysis (such as pharmaceutical water system data trends, clean area environmental monitoring trends, intermediate products and Finished product testing trends, etc.), through the identification and data accumulation of microorganisms monitored in the production environment (clean area and CNC area), raw materials, production personnel, and pharmaceutical water, provide data basis for the traceability analysis and investigation of contaminated microorganisms in the pharmaceutical production process , is an important content in the control of pharmaceutical microbial processes.
Some typical problems with detection in pollution control include:
① Insufficient control of the culture medium for sterility and microbiological testing. If the inspection finds that the finished product test thioglycolate fluid medium sample bottle (in the bacteria collector) in the on-site culture has been completely oxidized, and the medium for microbial limit testing has not been used to promote growth. test etc.
② Insufficient investigation and handling of over-standard and over-trend results, such as the failure of enterprises to properly investigate the root causes of reporting and recording false environmental monitoring results.
③ Failure to identify and effectively control abnormal trends or situations in the trend analysis of environmental monitoring or pharmaceutical water. For example, environmental monitoring found that surface microorganisms (1cfu/dish) were detected on the forehead of the clean clothes of the operators in the B-level filling room. The risk that the microorganisms on the surface of the clean clothes may eventually contaminate critical surfaces (such as in open vials) was not assessed, and the relevant batches were released; the microbial limit of water for injection was not detected to exceed the warning limit Analyze and evaluate.
④ The observation results of the environmental monitoring plate lack the review of the plate by other personnel.
Part 3 Conclusion
The core of the pollution control strategy is to establish a series of control measures and process control plans for the relevant elements of drug production quality management based on possible sources of pollution, and to clarify all key control points and control measures to avoid product contamination. Contamination control of sterile pharmaceuticals cannot rely solely on a certain control measure, it depends on a systematic pollution control strategy. Based on the analysis of the life cycle management and document requirements of the sterile drug contamination control strategy, this paper summarizes and refines the main pollution sources and typical defect examples in pollution control measures, which can further strengthen the drug contamination control for sterile drug manufacturers Provide reference, continuously reduce the risk of drug contamination, and continuously ensure the quality of drugs. At the same time, these typical problems are also relatively concentrated and easily overlooked contents in the pollution control of the production quality management of sterile drugs at home and abroad in recent years, and can also provide reference for the inspection of sterile drugs.