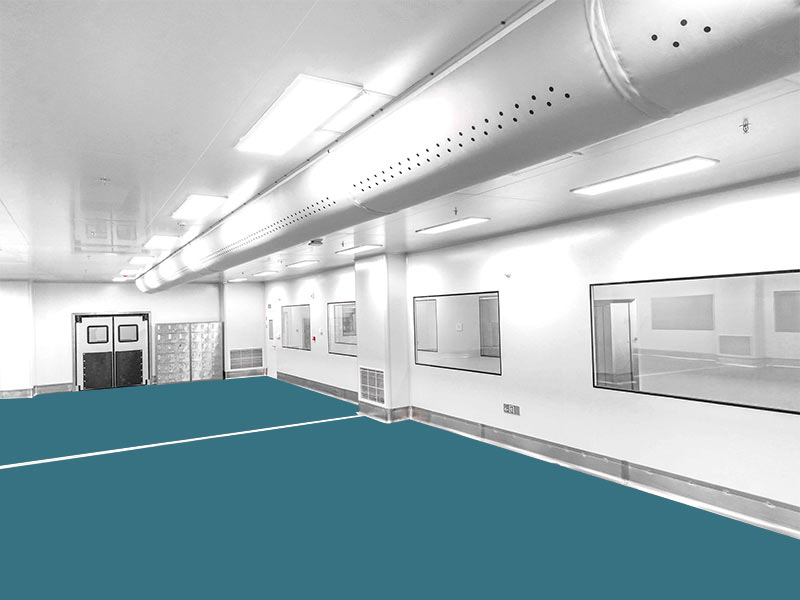
In the production of pharmaceuticals, the biggest source of pollution is the carrying of microorganisms when personnel enter and exit the clean area. Therefore, how to control personnel pollution and how to reduce the risk of drug contamination are the biggest problems facing pharmaceutical companies. At present, domestic pharmaceutical companies start with the design of the dressing room and the confirmation procedure of changing clothes to ensure the product quality of the drug.
1 The Purpose Of Changing Clothes In The Clean Area
(1) Protect the product from contamination by the operator, such as the operator’s skin and hair;
(2) Protect the product from the pollution of the external environment of the clean area, the main sources of pollution are work shoes, clothes, the entry of outdoor air in the clean room, etc.;

(3) Protect operators from being affected by the product;
(4) Reduce cross-contamination between different material boxes (or) products, and prevent products and materials adsorbed on clothes when leaving the clean area.
2 Key Points In The Design Of The Dressing Program In The Clean Area Of Aseptic Production
2.1 Material Selection And Quality Requirements For Clean Clothes
The selection of suitable clean clothes is the main means of prevention and control of pollution caused by personnel. In the pharmaceutical quality control specification, there are detailed regulations on the production of clothing materials for pharmaceutical companies: among them, it is required that the work clothes must be sterilized in one piece, and there must be no dropping or retention of fibers and particulate matter. There are two types of fabrics for work clothes, one is repeatable material, and the other is made of fiber in the form of spinning. The other is disposable materials, usually disposable materials are made of non-woven fabrics, it does not need to go through the spinning process. At the same time, the friction voltage requirement of clean clothes shall not exceed 300V, and it needs to have enhanced washing resistance.
2.2 Dressing Process Design Standards
The design of sterile changing facilities is the hardware guarantee of the changing procedure and plays an extremely important role. Our country currently has different personnel flow design schemes for sterile pharmaceutical companies, but they all abide by the basic principles.
(1) The size of the changing room should be adapted to the number of people who need to change at the same time;
(2) Changing areas and facilities shall be provided in the changing room for personnel to store coats, change shoes, wash hands (disinfect), and change clean clothes. Personnel coats and clothing shall not be brought into Class B or C clean areas;
(3) For A and B-level clean areas, sterile clean work clothes must be replaced every time they enter. Enterprise aseptic workshops must meet the maximum load of cleaning and sterilization work clothes. If the pharmaceutical company requires that the sterile clean work clothes be changed at least once per shift, it is necessary to set up clothes storage racks and shoe changing stools in the changing room for personnel to avoid contamination of the clothes on the ground during the process of taking off and changing the clean clothes;
(4) Frequently replace the disinfection masks and gloves. Channels set up areas for changing masks and gloves;
(5) For the locker rooms for those who produce highly allergic drugs such as penicillin, some steroid drugs, highly active drugs and toxic drugs, purification measures should be taken to prevent toxic and harmful substances from being taken out by the human body, such as setting up two locker rooms for advancing and retreating respectively. When personnel enter, the clean changing room adopts a positive pressure air chamber to prevent the active materials or products in the production area from flowing into the changing room. Active materials or products on the outflow locker room;
(6) There should be enough air changes in the changing room, and the static level of the back section of the sterile changing room should be the same as that of other corresponding clean areas, for example, the lowest level should reach level B;
(7) Entering and leaving the sterile area should adopt different routes through the changing room to avoid contamination of the sterile environment and sterile clothing. At the same time, pay attention to the distribution channel of the clean clothes before entering and the recovery setting of the clean clothes after leaving. Remember that the clean work clothes of A and B grades can only be used once after sterilization at this time;
(8) Necessary mirrors should be set up in the dressing room, and signs and icons should ensure that personnel can dress correctly;
(9) The two doors of the dressing room shall be designed to be interlocked to prevent the opening of the other door when one door is not fully closed. This interlock shall be automatically disabled in the event of a fire alarm;
(10) Changing rooms cannot be used to transport products, materials, or equipment between areas.
2.3 Personnel Training And Assessment
For entering the aseptic pharmaceutical workshop, the requirements for the changing procedure of level A and level B are particularly cumbersome, and this is also the basic requirement to ensure the successful verification of the changing procedure. Pharmaceutical companies can gain training effectiveness by using diverse training methods. Such as: student drills, playing a model video of changing procedures, etc., to lay the foundation for the trainees to enter the changing procedure in the production clean area.
3 Verification Points Of Changing Procedures In Clean Area Of Aseptic Production
In the clean area, the flow of people is one of the most serious sources of pollution. Therefore, strict supervision of employee changing procedures and minimizing the bacteria carried by employees are the basis for ensuring that the clean area remains clean. When entering and leaving the clean area, employees should carry out strict changing procedures. Especially in Class B clean areas, it is necessary to provide training on the changing process for employees who frequently enter and exit, and simulate the process of changing clothes in and out of clean areas to ensure that employees in Class B clean areas are more proficient in entering and exiting the changing procedures, and reduce the number of microorganisms on the body surface of employees, thereby Reduce the risk of product contamination.
3.1 Confirmation Procedure
(1) Each trainee must be trained in aseptic operation in advance, such as SOP for wearing sterile gowns, contact sampling method, contamination control and aseptic operation techniques, etc.;
(2) Before entering the aseptic production cleanliness, the trainees must first practice changing clothes;
(3) Managers must explain to each trainee the procedures for monitoring of changing surfaces;
(4) Use surface monitoring for 3 dressing procedures;
(5) The direct contact method or the cotton swab method shall be used for sampling each surface monitoring, and the rationality of the sampling point shall be explained.
3.2 Frequency
(1) Each first-time trainee must pass 3 times of changing clothes before entering the clean area of sterile production. Especially for the operators in the Class B clean area, the scope of work does not involve the simulated filling operation of the medium, so even employees who have not participated in the training of the simulated filling operation of the medium, as long as they pass the confirmation of changing clothes, they can Work in this area. However, when working in a Class B clean area, because it involves the simulated filling operation of the culture medium, the personnel entering this area must not only pass the aseptic changing procedures to confirm, but also need to pass the simulated culture medium filling to be able to enter;
(2) Those who have passed the dressing test shall repeat the dressing test once a year;
(3) When it is found that qualified personnel have a tendency to violate the dressing procedure, it is necessary to re-check the dressing procedure.
3.3 Eligibility Criteria For Changing Clothes
(1) It has been demonstrated that the trainee has mastered the procedures of changing clothes, contamination control and aseptic technique;
(2) The data and video show that the procedures of the trainee’s three dressing tests are correct;
(3) The microbiological test results of the test are within the acceptable standard.
3.4 Detection Of Bacteria Carrying Amount In Sterile Clean Clothes
Bacterial carrying amount detection of sterile clean clothes in Class B clean area needs to extract bacterial samples twice, before the staff enters the clean area for operation, and samples are also taken when the staff completes the work and leaves the clean area.
The detection method is as follows: swab the staff’s wrists, fingers of both hands, head, shoulders, forearms, eye masks, masks, and foot covers with cotton swabs to take samples, and use the contact disc method to sample when leaving the clean area.
4 Summary
The verification procedure for dressing personnel in the clean area of aseptic production is to ensure the quality of drugs and is the most critical procedure for aseptic production of drugs. If pharmaceutical companies want to ensure the aseptic production of drugs, they must train personnel, strictly supervise the changing process and verification of employees, and ensure the normal use of hardware facilities in order to achieve safe drug production.